What To Know About Mammograms And Breast Health
Key Takeaways:
- Regular mammograms are crucial for early detection of breast cancer.
- Recent guidelines recommend starting screenings at age 40.
- Understanding breast density can influence screening decisions.
- Advancements in AI are enhancing the accuracy of mammograms.
The Importance of Regular Mammograms
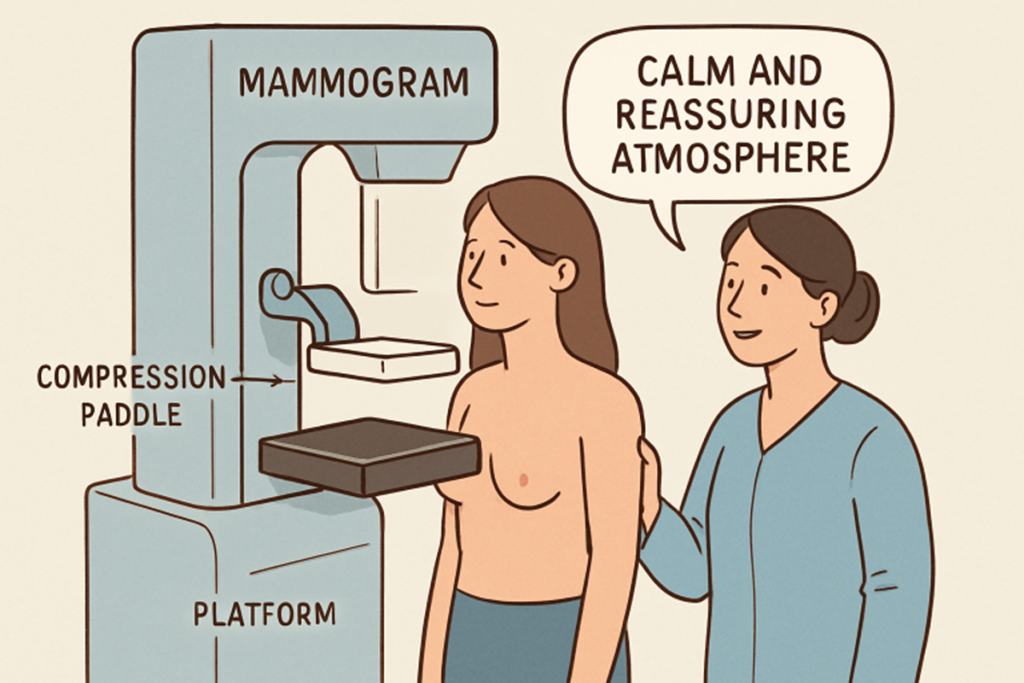
Taking proactive steps toward breast health is one of the most important things women can do for their long-term well-being. Regular mammograms are the cornerstone of early breast cancer detection, offering an opportunity to find abnormalities well before they manifest as symptoms. By identifying cancer at its earliest, most treatable stages, mammograms can save lives and minimize the need for aggressive treatments. If you’re seeking experienced and compassionate care, consider scheduling your screening at a Boise mammography screening clinic.
National health organizations emphasize the importance of mammograms. Early detection through screening is vital, significantly enhancing treatment success and survival odds for breast cancer patients.
Updated Screening Guidelines
In recent years, a notable shift has occurred in mammogram guideline recommendations. Due to a rise in breast cancer rates among younger women, the U.S. Preventive Services Task Force has updated its advice: women should now begin regular mammogram screenings at age 40, continuing every two years up to age 74. This adjustment is significant for those in higher-risk groups, aiming to address disparities in outcomes and help close the gap in early detection. For more background on these changes, visit the coverage.
Regular and timely screenings empower women to take charge of their breast health—an especially vital step for individuals with family histories of breast cancer or other significant risk factors. This commitment to proactive health management is underscored by leading cancer specialists and healthcare providers nationwide.
Understanding Breast Density
Another factor that can impact mammogram accuracy and breast cancer risk is breast density. Women’s breasts are made up of varying proportions of glandular, connective, and fatty tissue. Those with more fibrous and glandular tissue have “dense breasts,” which can make it difficult for mammograms to distinguish cancerous areas from normal tissue. Not only does this complicate diagnosis, but higher breast density itself is also associated with an increased risk of developing breast cancer. According to data from the , understanding these statistics can help women make informed decisions about screening and preventive care.
Including breast density information in mammogram reports allows women to consider additional imaging or alternate strategies when appropriate, supporting more informed conversations between patients and healthcare providers.
Advancements in Mammography Technology
Mammography technology is evolving at a rapid pace, with exciting breakthroughs that are improving detection and diagnosis. Artificial intelligence (AI) and advanced digital imaging are now playing an increasingly important role in analyzing mammogram results. Recent research indicates that AI can detect subtle, potentially cancerous changes in breast tissue over time, sometimes before they become visible to a radiologist’s eye. These improvements offer hope for even earlier—and more accurate—diagnoses.
Leading healthcare systems nationwide are integrating these technologies to enhance patient care and minimize human error. For a deeper dive into how AI is reshaping breast cancer detection, see coverage in These technological improvements are also enabling more personalized screening plans based on a patient’s individual risk. As these tools continue to evolve, patients can look forward to faster, more accurate, and customized approaches to detecting breast cancer.
Addressing False Positives
A common concern related to mammograms is the risk of false positives—when a mammogram suggests the presence of cancer that further testing disproves. False positives can cause anxiety, lead to unnecessary procedures, and, in some cases, discourage women from returning for future screenings. However, the benefits of early detection overwhelmingly outweigh these temporary setbacks.
Open and continuous communication with healthcare providers is essential for understanding the relative risks and benefits. By staying informed and asking questions, women can make empowered choices regarding their screening schedules and reduce the anxiety often associated with false alarms.
Personalized Screening Plans
Breast cancer screening isn’t a one-size-fits-all process, as individual risk levels can vary widely. Factors like genetics, family history, previous biopsies, and overall health all influence the most appropriate screening strategy. Experts often suggest that women have annual conversations with their healthcare providers to assess any changes and adjust their screening plans accordingly.
Customized screening approaches help ensure that each woman receives care suited to her specific risk profile. This may involve additional imaging, genetic counseling, or initiating screenings earlier and conducting them more frequently for individuals at higher risk. Staying informed and proactive enables women to make decisions that support their long-term health. At the same time, open communication with healthcare providers helps balance the benefits and potential risks associated with screening. For more information on tailoring a screening plan, the offers helpful resources. Regularly reviewing your risk factors and screening schedule helps detect potential issues early. Taking a proactive approach empowers women to take control of their health with confidence.
Staying Informed and Proactive
Establishing an intense breast health routine and staying up to date with the latest screening guidelines can make a significant difference in outcomes. Regular self-exams, awareness of personal risk factors, and adherence to recommended mammogram schedules are all elements of a comprehensive strategy. Advances in technology and greater access to critical information have empowered women to take greater control of their care.
In summary, understanding the importance of mammograms, setting appropriate screening intervals, and leveraging advances in technology are crucial steps in safeguarding breast health. By being informed and proactive, women can increase their chances of early detection, enhance treatment outcomes, and experience greater peace of mind.




