CANCER Diagnosis and Staging: A Complete Guide to Understanding the Process
Cancer is one of the most challenging health conditions worldwide, affecting millions of individuals and families each year. Early detection and accurate staging play a critical role in determining the most effective treatment plan and improving survival outcomes. Understanding how cancer is diagnosed and staged can help patients and their loved ones feel more informed, prepared, and confident when navigating this journey.
In this comprehensive guide, we’ll explore the essential aspects of CANCER Diagnosis and Staging, including common diagnostic tools, staging systems, and why precision in both areas is crucial for personalized treatment planning.
What Is Cancer?
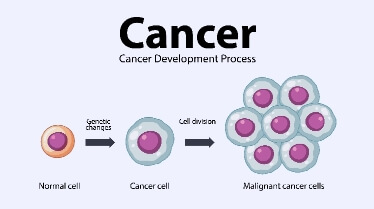
Cancer refers to a group of diseases characterized by uncontrolled cell growth. Normally, cells grow, divide, and die in an organized manner. However, when this process becomes disrupted, abnormal cells can multiply rapidly and form tumors. Some cancers remain localized, while others spread (metastasize) to different parts of the body.
Because each type of cancer behaves differently, accurate diagnosis and staging are essential to determine its severity and the most appropriate treatment options.
Why Early Cancer Diagnosis Matters
Early diagnosis significantly increases the chances of successful treatment. When cancer is detected at an early stage:
- Treatment options are often less aggressive
- Survival rates are higher
- Complications may be minimized
- Quality of life can be better preserved
Modern medical centers like Liv Hospital emphasize advanced diagnostic technologies and multidisciplinary care to ensure accurate and timely cancer detection.
Understanding CANCER Diagnosis and Staging
The process of CANCER Diagnosis and Staging involves two main steps:
- Confirming whether cancer is present
- Determining how far it has spread
Both steps are essential in developing a personalized treatment plan.
Step 1: Cancer Diagnosis
Cancer diagnosis involves several methods and tests. Physicians select specific diagnostic tools depending on symptoms, medical history, and suspected cancer type.
1. Medical History and Physical Examination
The diagnostic process often begins with:
- Reviewing symptoms
- Assessing family history
- Conducting a physical examination
Certain warning signs—such as unexplained weight loss, persistent fatigue, unusual bleeding, or lumps—may prompt further testing.
2. Imaging Tests
Imaging technologies help doctors visualize internal organs and detect abnormalities.
Common imaging tests include:
- X-rays – Detect bone abnormalities and some lung cancers
- CT (Computed Tomography) scans – Provide detailed cross-sectional images
- MRI (Magnetic Resonance Imaging) – Ideal for soft tissue imaging
- PET (Positron Emission Tomography) scans – Identify cancer activity
- Ultrasound – Useful for abdominal and pelvic evaluation
These imaging methods help determine tumor size and location.
3. Laboratory Tests
Blood and urine tests can reveal abnormal markers that may indicate cancer. Examples include:
- Tumor markers (e.g., PSA for prostate cancer)
- Complete blood count (CBC)
- Liver and kidney function tests
While laboratory tests alone cannot confirm cancer, they support further diagnostic decisions.
4. Biopsy – The Definitive Diagnosis
A biopsy is the most reliable method for confirming cancer. During this procedure, a small tissue sample is removed and examined under a microscope by a pathologist.
Types of biopsy include:
- Needle biopsy
- Surgical biopsy
- Endoscopic biopsy
- Bone marrow biopsy
The biopsy not only confirms the presence of cancer but also identifies the specific type and grade.
Understanding Cancer Staging
Once cancer is diagnosed, staging determines the extent of its spread. Staging is critical because it:
- Guides treatment decisions
- Predicts prognosis
- Allows comparison of treatment outcomes
- Facilitates communication among healthcare professionals
The TNM Staging System
The most widely used cancer staging method is the TNM system:
- T (Tumor): Size and extent of the primary tumor
- N (Nodes): Whether cancer has spread to nearby lymph nodes
- M (Metastasis): Whether cancer has spread to distant organs
Each category receives a number or letter to describe severity.
For example:
- T1 indicates a small tumor
- N0 means no lymph node involvement
- M1 indicates distant metastasi
Cancer Stages (0–IV)
Based on TNM classification, cancers are grouped into stages:
Stage 0
Cancer cells are present but have not spread beyond their origin (in situ).
Stage I
Cancer is small and localized.
Stage II & III
Cancer has grown larger and may have spread to nearby lymph nodes.
Stage IV
Cancer has spread to distant organs (advanced or metastatic cancer).
The stage significantly influences treatment strategies.
How Staging Affects Treatment Decisions
Cancer treatment plans are highly individualized. Based on diagnosis and stage, doctors may recommend:
- Surgery
- Chemotherapy
- Radiation therapy
- Immunotherapy
- Targeted therapy
- Hormone therapy
For early-stage cancers, surgery alone may be sufficient. Advanced stages often require a combination of treatments.
Specialized oncology centers focus on multidisciplinary approaches where oncologists, radiologists, pathologists, and surgeons collaborate to create personalized care plans.
Advanced Technologies in Cancer Diagnosis
Modern healthcare facilities utilize cutting-edge technology to improve diagnostic accuracy, including:
- Molecular testing
- Genetic profiling
- Liquid biopsy
- AI-assisted imaging
- Precision oncology tools
These advancements allow physicians to tailor treatments according to the unique genetic characteristics of a tumor.
Emotional and Psychological Aspects of Diagnosis
Receiving a cancer diagnosis can be emotionally overwhelming. Common reactions include:
- Anxiety
- Fear
- Confusion
- Depression
Comprehensive cancer care should include psychological support, counseling, and patient education to help individuals cope effectively.
The Importance of Multidisciplinary Care
A team-based approach improves patient outcomes. A multidisciplinary cancer care team may include:
- Medical oncologists
- Surgical oncologists
- Radiation oncologists
- Radiologists
- Pathologists
- Oncology nurses
- Psychologists
This collaborative method ensures all aspects of the disease are addressed.
Follow-Up and Monitoring
Even after treatment, regular follow-up is crucial. Monitoring includes:
- Imaging tests
- Blood tests
- Physical examinations
- Symptom tracking
Early detection of recurrence increases the likelihood of successful management.
Frequently Asked Questions (FAQs)
1. How long does cancer diagnosis take?
The timeframe varies depending on the type of cancer and required tests. It may take several days to a few weeks.
2. Can cancer be diagnosed with a blood test alone?
No. Blood tests can suggest abnormalities, but a biopsy is usually required for confirmation.
3. Is Stage IV cancer always terminal?
Not necessarily. Many Stage IV cancers can be managed for years with modern treatments.
4. Does staging change over time?
The original stage at diagnosis does not change, but cancer progression or recurrence is documented separately.
5. Can early-stage cancer be cured?
Many early-stage cancers can be successfully treated, especially when detected promptly.
Final Thoughts
Understanding cancer diagnosis and staging empowers patients to participate actively in their treatment journey. Accurate detection, proper staging, and personalized care are the foundation of effective cancer management. Advances in medical technology continue to improve survival rates and treatment outcomes worldwide.
Beyond medical treatment, maintaining a healthy lifestyle and focusing on overall well-being can positively influence recovery and resilience. For guidance on balanced living, wellness tips, and improving quality of life, you can explore helpful resources at live and feel, where health-conscious living meets practical everyday inspiration.





